by the World Health Organization (WHO), with two variants of the disease spreading around the world, one of which has far more severe effects.
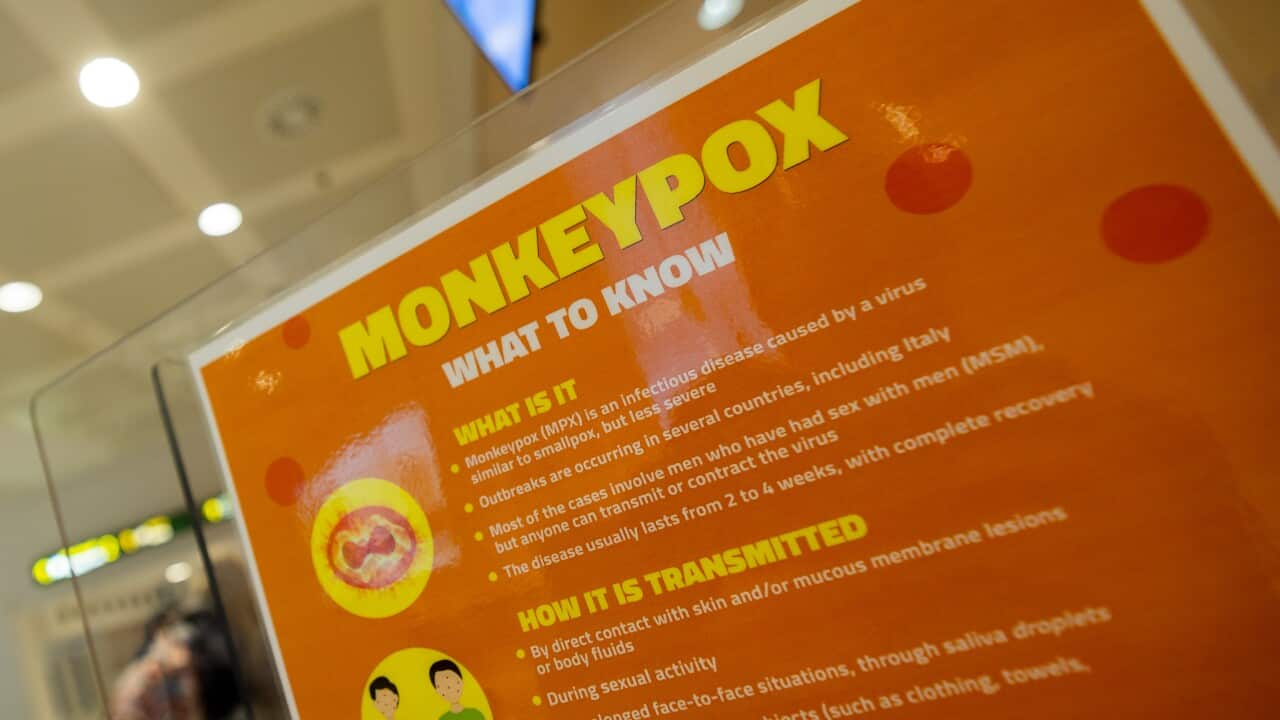
Mpox, previously known as monkeypox, is an infectious disease caused by a virus that can cause a painful rash, enlarged lymph nodes and fever.
It was first discovered in 1958 in monkeys kept for research in Denmark and the first human case was reported in the Democratic Republic of the Congo in 1970.
Anyone can get mpox, which spreads through touch or sexual contact with infected people, hunting or cooking infected animals and contact with infected materials such as sheets or needles.
It can also be passed on to unborn babies during pregnancy.
Mpox can cause severe sickness and complications including the skin becoming infected with bacteria, pneumonia, corneal infection with loss of vision, vomiting and diarrhoea causing severe dehydration or malnutrition and sepsis (infection of the blood).
While mpox is generally not life-threatening, some people are more likely to get severely ill, including people with severely weakened immune systems, children under one year old, people with a history of eczema and pregnant people.
Types of mpox
There are two major variants (or clades) of mpox: clade 1 and clade 2.
Clade 1 causes more severe illness and deaths and previous outbreaks have killed up to 10 per cent of the people who get sick — although more recent outbreaks have had lower death rates.
Clade 2 causes a less severe infection and more than 99.9 per cent of those infected survive.

The clade 1 variant of mpox has now been detected in 12 African countries. Source: Getty, AFP / Tchandrou Nitanga
Clade 2 mpox is endemic to West African nations, including Sierra Leone, Liberia and Nigeria.
The recent spread of mpox
The current outbreak of mpox, caused by a variant known as clade 1b in Central Africa, started in the Democratic Republic of the Congo in late 2023.
Clade 1b of mpox is particularly concerning for public health authorities as it seems to have higher transmissibility and potential for severe clinical outcomes than many previous subvariants.
As of 16 August, there have been at least 18,700 mpox cases and 541 deaths across 12 African countries since the beginning of the year, according to the Africa Centres for Disease Control and Prevention (CDC).
Burundi, Central African Republic, Rwanda and Uganda are among the affected countries.
While previous outbreaks of , the 2024 outbreak is impacting a broader demographic of people.
The Democratic Republic of the Congo accounts for 95 per cent of the reported cases and 99 per cent of deaths, making it the main focus of the response.
Mpox was declared a Public Health Emergency of Continental Security on 13 August by Africa CDC director-general Jean Kaseya. This was the first declaration of its kind by Africa CDC.
A day later, it was declared a Public Health Emergency of International Concern by WHO's director-general Tedros Adhanom Ghebreyesus.
On 15 August, global health officials confirmed the new clade 1b strain had been detected in Sweden after a traveller returned from Africa.
This week, Thailand also confirmed a case of the clade 1b strain of the virus, which had infected a 66-year-old man from a European country who had arrived in Thailand last week from an unspecified African country where the disease was spreading.
Thai authorities said on Wednesday the man had transited through a Middle Eastern country, which was also not named, before flying on to Thailand.
The clade 2 spread
There is a concurrent spread of mpox clade 2 across the globe that has been happening since 2022.
The variant spreading is a subclade known as 2b.
While WHO declared this outbreak a public health emergency of international concern in July 2022, the emergency classification was lifted in May 2023 due to a significant decline in cases and control measures instituted by countries such as vaccinations and transmission monitoring.
In Australia, there's been a significant uptick in cases since the beginning of 2024, as compared to the number of cases reported in 2023.
This mpox variant has been detected in NSW, Victoria and Queensland, with a total of 314 cases reported as of 24 August.
In 2023, only 26 cases were reported in total in Australia.
The Department of Health says most people don't require treatment for mpox beyond simple pain relief. However, antiviral treatment may be needed in patients with more severe disease.
Vaccines can also be given either before or after a person is exposed to the virus — but before exposure is recommended for the best protection.
However, due to the high global demand for the mpox vaccine, access in Australia is being prioritised for high-risk groups.
These include people who are in close physical contact with others infected with mpox, groups at higher risk of exposure such as gay and bisexual men or other men who have sex with men, healthcare and laboratory workers, or those travelling to countries where mpox is present.
The response to mpox in Africa
WHO have responded swiftly to the mpox clade 1 outbreak, calling on UN member states to increase their preparedness and readiness capacities, boosting surveillance of the disease, improving specimen collection and transportation, and helping countries to develop vaccine strategies.
While the mass vaccinations seen during the COVID-19 pandemic are not currently recommended, African nations currently require around 10 million doses of vaccines but only around 200,000 are available.
WHO, Africa CDC and Gavi, the Vaccine Alliance have entered discussions with manufacturers to try and meet needs and WHO has called for vaccine candidates to have fast approval and distribution.