Australia is , seeing increasing cases, more hospitalisations and a greater number of prescriptions for COVID-19 antivirals dispensed over recent months.
In the early days of the pandemic, the only medicines available were those that treated the symptoms of the virus. These included steroids and analgesics such as paracetamol and ibuprofen to treat pain and fever.
But are these drugs effective against current variants? And who is eligible to receive them? Here’s what to know about antivirals as we navigate this eighth COVID-19 wave.
What antivirals are available?
Paxlovid is a combination of two different drug molecules, nirmatrelvir and ritonavir. The nirmatrelvir works by blocking an enzyme called a protease that the virus needs to replicate. The ritonavir is included in the medicine to protect the nirmatrelvir, stopping the body from breaking it down.
Molnupiravir, marketed as Lagevrio, works by forcing errors into the RNA of SARS-CoV-2 () as it replicates. As these errors build up, the virus becomes less effective.

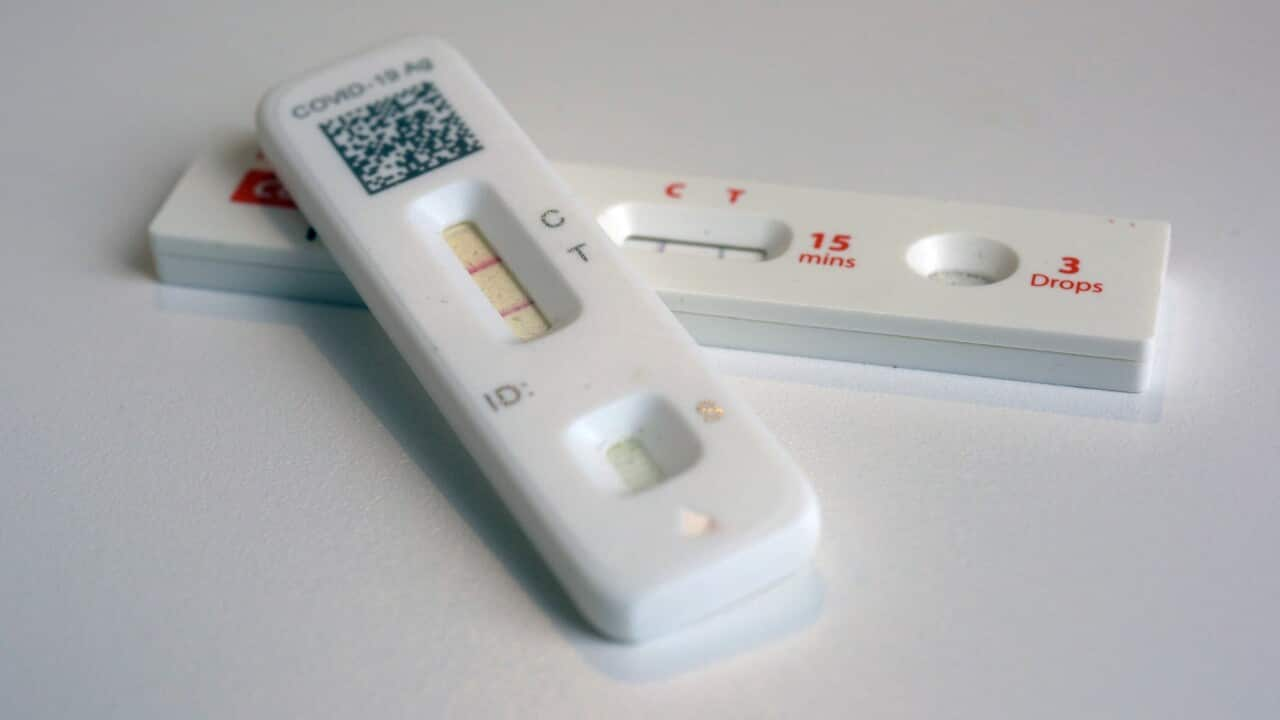
Paxlovid is one of two drugs available that treat the virus that causes COVID-19. Source: AAP, SIPA USA / Richard B. Levine
This is different to the monoclonal antibody-based medicines that were developed against specific strains of the virus. These drugs are not thought to be effective for any variant of the virus from onwards, which includes the current wave. This is because these drugs recognise certain proteins expressed on the surface of SARS-CoV-2, which have changed over time.
What does the evidence say?
As Lagevrio and Paxlovid are relatively new medicines, we’re still learning how well they work and which patients should use them.
The latest evidence suggests Paxlovid decreases the risk of hospitalisation if taken early by those at the highest risk of severe disease.
Results from a previous trial suggested Lagevrio might reduce COVID-19 deaths. But a more recent, larger trial indicated Lagevrio doesn’t significantly reduce hospitalisations or deaths from the virus.
However, few people at the highest risk from COVID-19 were included in this trial. So it could offer some benefit for patients in this group.

Older adults are among those eligible for COVID antivirals. Source: Getty / fcafotodigital
Paxlovid also can’t be taken alongside some other medications such as those for certain heart conditions, mental health conditions and cancers. For high-risk patients in these cases, Lagevrio can be considered.
Some people who take COVID antivirals will experience side effects. Mostly these are not serious and will go away with time.
Both Paxlovid and Lagevrio can cause diarrhoea, nausea and dizziness. Paxlovid can also cause side effects including muscle aches and weakness, changes in taste, loss of appetite and abdominal pain. If you experience any of these, you should contact your doctor.
More serious side effects of both medicines are allergic reactions, such as shortness of breath, swelling of the face, lips or tongue and a severe rash, itching or hives. If you experience any of these, call 000 immediately or go straight to the nearest emergency department.
Be prepared
Most people will be able to manage COVID-19 safely at home without needing antivirals. However, those at higher risk of severe COVID-19 and therefore eligible for antivirals should seek them. This includes people aged 70 or older, people aged 50 or older or Aboriginal people aged 30 or older with one additional risk factor for severe illness, and people 18 or older who are immunocompromised.
If you are in any of these groups, it’s important you plan ahead. Speak to your healthcare team now so you know what to do if you get COVID-19 symptoms.
If needed, this will ensure you can start treatment as soon as possible. It’s important antivirals are started within five days of symptom onset.
If you’re a high-risk patient and you test positive, contact your doctor straight away. If you are eligible for antivirals, your doctor will organise a prescription (either an electronic or paper script).
These medicines are available under the Pharmaceutical Benefits Scheme (PBS) and subsidised for people with a Medicare card. The cost for each course is the standard. PBS co-payment amount: $30 for general patients and $7.30 for people with a concession card.
So you can rest and reduce the risk of spreading the virus to others, ask your pharmacy to deliver the medication to your home, or ask someone to collect it for you.
Dr Jessica Pace is an associate lecturer at Sydney Pharmacy School, University of Sydney.
Nial Wheate is an associate professor of the Sydney Pharmacy School, University of Sydney.