Loody Stewart's son Charles died at the age of 27 from cystic fibrosis.
Ms Stewart said her son, who was diagnosed with the genetic condition as a baby, was incredibly grateful to be able to spend his final months in palliative care at home surrounded by his loved ones.
Palliative care helps terminally ill patients with their physical, emotional, spiritual and social needs. It can be provided at home, in hospitals or in aged care facilities.
"What made his last six months incredibly powerful, or empowered Charles, is the fact that he received palliative care at home," Ms Stewart said.
"It meant he was able to be not just with immediate family but his close friends, extended family, in his home environment with his pets."
But palliative care did not just bring comfort to her loved one who was dying, Ms Stewart said.
She said his care also helped her and her family leading up to and after Charles' death.
"It's difficult to put into words. It was very precious. The thing is it's not only precious in those six months," Ms Stewart said.
"It's an ongoing journey for anyone who has had a family member or friend go through palliative care and they think after that person passes... they sort of think, 'Oh well, it's all done and dusted'.
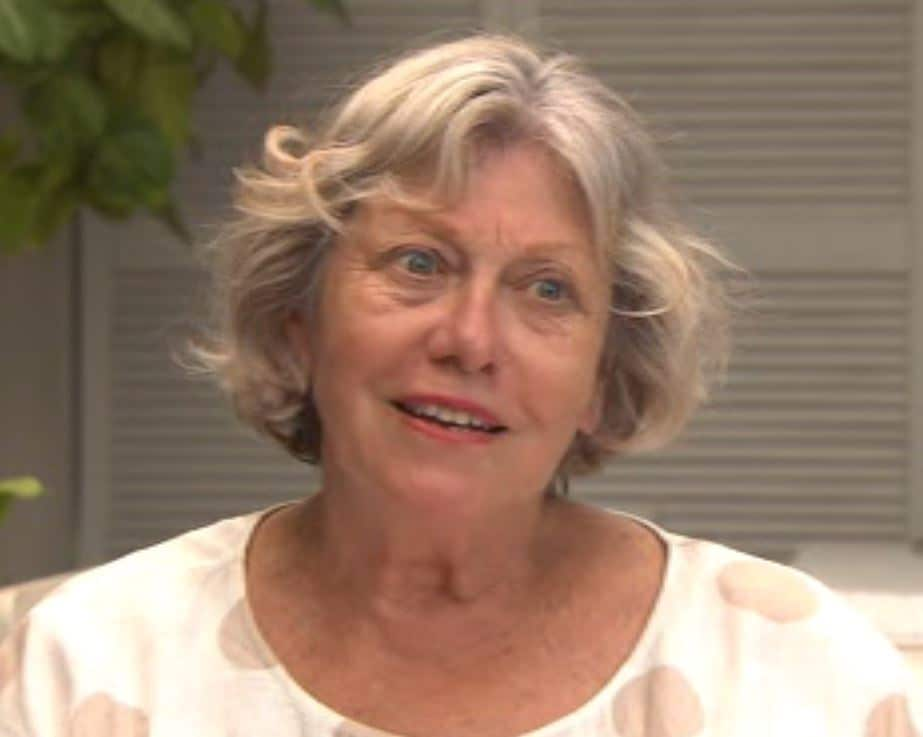
Loody Stewart's son Charles died at the age of 27 from cystic fibrosis. He received palliative care in the last months of his life. Source: Seven Network
"That's just a beginning of another journey. This is where the palliative care just helped exponentially. They supported me and my family on Charles' journey.
"It's nearly two years now [since her son's death] but they also gave us the opportunity now I can reflect on Charles' journey. And every day I would reflect on a conversation with Charles I had at home.
"I reflect on the last 24 hours when we knew Charles was going to pass away. But his twin brother... was with him, I was with him, his close friends had visited, and that has given me enormous strength."
Ms Stewart is advocating for more funding as the nation's peak body for palliative care says the system is under pressure.
Palliative Care Australia chief executive officer Liz Callaghan says many Australians are not able to access services.
"There's a shortfall of around 60,000 Australians who could potentially benefit from palliative care, accessing palliative care services who don't," she said.
According to Palliative Care Australia, there is just one medical specialist for every 704 deaths each year.
In a statement, Aged Care Minister Ken Wyatt said the government was working with all states and territories to develop a national palliative care strategy.
He also said more than $82 million would be spent on palliative care over the next three years.
Ms Callaghan says while this indicates good intentions, more needs to be done.
"It's a very good signal to the sector that there is strong support from the government for palliative care but it falls very short of what's needed," she said.
"So state and territory governments also need to match that investment."
There are calls for a national palliative care commissioner to address gaps in services that can see rural and multicultural patients disadvantaged in particular.
Last year Brisbane-based hospice service Karuna had to turn patients away for the first time in 25 years.
Karuna Hospice Services Board chair Catherine Mickel says many nurses are feeling the pressure.
"Certainly there has been a quantum change in Australian society and now we are seeing that there is a demand that can't be met," she said.
"So we absolutely need more funding to provide the resources so that we can better meet the need."
Ms Stewart said the support she received from her son's palliative carers helped with her grieving process.
"You can't put a dollar figure on it but it's enormously important. And for the ongoing health of those that have been with that person in palliative care it just greatly reduces the stress level of the person when they know they're heading towards end of life," she said.
"I wish someone in the government could come and spend time in the home of someone going through palliative care and realise how incredibly important and incredibly special it is and it's not just that point in time it's the ongoing effect on those close to that person."










