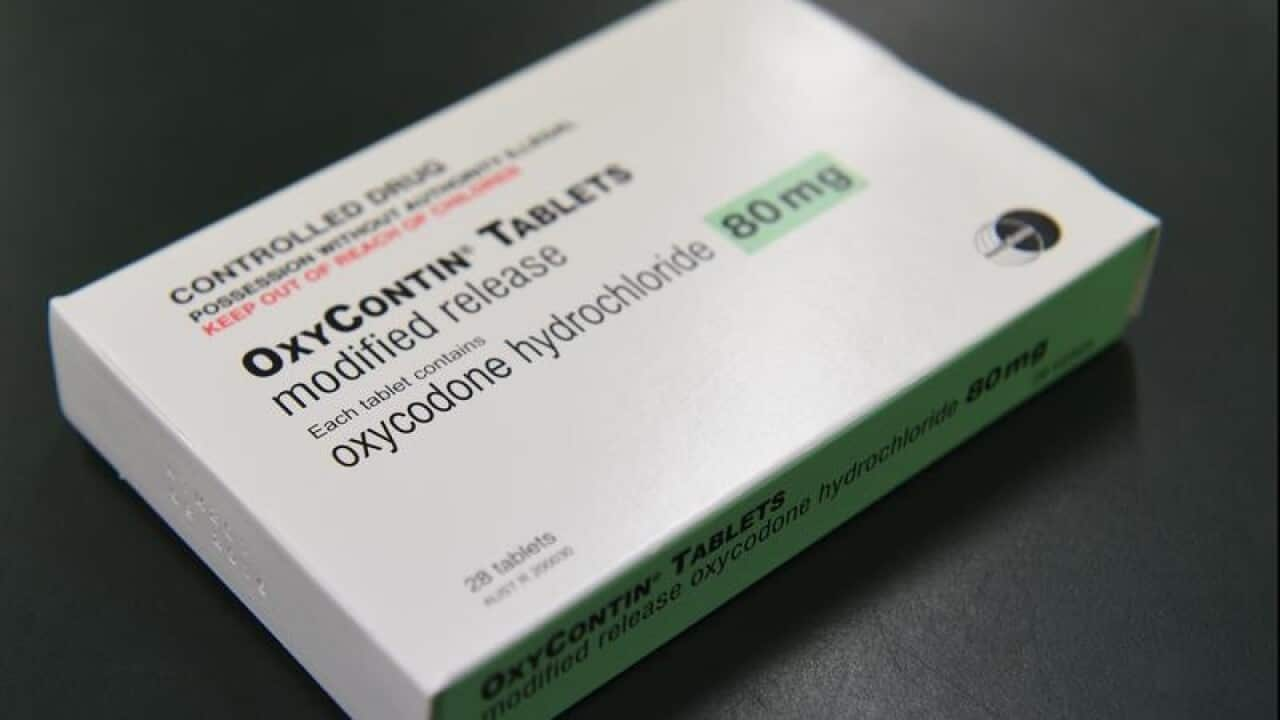
Australian doctors, particularly those who work in hospitals, have been warned about the potentially fatal risks of prescribing slow-release opioids like oxycodone and fentanyl patches.
In response to the global opioid epidemic, the Australian and New Zealand College of Anaesthetists (ANZCA) and its Faculty of Pain Medicine has written to 34 leading medical colleges and associations including the Royal Australian College of General Practitioners and the Royal Australasian College of Physicians to advise against prescribing these medications for acute pain.
"It seems to us that the community is literally being flooded with prescription opioids," said ANZCA President, Professor David A Scott.
Of particular concern to ANZCA is the prescription of slow-release opioids.
"It's become apparent from coroner's reports about adverse patient outcomes that in particular slow-release opioids are being used inappropriately or continued on indefinitely once they are discharged from hospitals," Prof Scott said.
All opioids cause sedation and slow a person's breathing. The problem with slow-release opioids, explains Prof Scott, is that they remain in the system for "hours and hours".
"They're not just wearing off gradually," Prof Scott said.
This increases a person's risk of adverse side-effects, including respiratory depression and even death, warns ANZCA.
First-time users, the elderly and people on other medications are at greatest risk of side-effects.
The other concern is that people are vulnerable to developing a dependence on these medications.
"We know that if you are discharged home with slow-release opioids, there is a strong chance you'll still be taking those opioids a year later, and that's just because the script keeps getting repeated and no-one actually changes it," Prof Scott said.
In Australia, more people now die from the misuse of prescription opioids than they do from heroin overdose.
Prof Scott said anaesthetists and specialist pain medicine physicians need to show leadership of this "serious issue" and control the use of these potent and potentially toxic painkillers.
"It's not to say opioid painkillers aren't useful, they can be very useful but we are stressing they should only be used for the shortest period of time necessary," he said.
"If you need to use an opioid painkiller, make it a short-acting one, so you can adjust the dose to the patient's needs."
The college also advises its specialists to reassess opioid prescription on discharge from hospital.
Prof Scott said patients should not be discharged from hospital with a full pack of these medications but instead just enough for a few days.
"Send them off with a limited dose and a clear plan, that is the message," he said.