Key Points
- Mpox is on the rise in Australia, with more than 275 cases recorded in September as of Friday.
- The virus was declared a public health emergency by the World Health Organization in August
- Experts say those eligible should get vaccinated.
Mpox has been increasingly spreading in parts of the world for the past two years, but cases in Australia have remained low.
Now, numbers are surging, with more than 600 reported in the current quarter compared with only six in the first three months of the year.
The virus was declared a public health emergency by the World Health Organization in August, and experts say those at risk of infection should remain vigilant.
Here's what we know.
Is mpox increasing in Australia, and should we be concerned?
According to the government's National Notifiable Disease Surveillance System, there have been 748 cases reported in 2024 at the time of writing. In 2023, there were a total of 26 cases.
NSW and Victoria have had the most cases, with 407 and 255 respectively. Queensland has reported 61 cases, while the ACT has reported 15.
South Australia and Western Australia have reported seven and two cases respectively, while the Northern Territory has had one. Tasmania is the only jurisdiction with no cases.
CSIRO Health and Biosecurity virologist Dr Nias Peng said while rising case numbers are not cause for panic, they should be taken seriously.
"I think it's something that Australians should be concerned about but not be freaking out," he said.
"Remain vigilant and be aware of the symptoms and how it is able to transmit and spread between people."
Peng said he believes the virus has been underestimated in Australia.
"It seems like the general consensus among the public is that it's not a big deal so far," he said.
"But that's the wrong thing to assume ... because that's how you eventually get a massive spread of diseases among the population."
Dr Matt Mason, lecturer in nursing at the University at the Sunshine Coast, said for some members of the community at risk of infection — such as men who have sex with other men — accessing medical care can also be an issue.
"What we're seeing is this increase in mpox in a particular population and this population is marginalised," he said.
"When people have a good relationship with their medical provider, most people are getting vaccinated, but there is a significant proportion that aren't because there is a lack of trust in the health system."
He said some people might not be comfortable seeking healthcare or vaccines if they have previously had bad experiences with the medical system.
"The vaccines are available here in Australia, and we do have a very good sexual health network, but the issue is getting people to access it," he said.
"Particularly the groups of men who are sex with men have been not well looked after in the past by the health system, so there is some stigma there, particularly if people don't identify as homosexual, they don't feel that they fit into that sort of category."
As of Friday, 275 mpox cases had been recorded in September, a new monthly peak for Australia.
The vast majority of the 2024 cases are among men, with only three women diagnosed.
Most new cases have been locally transmitted, rather than people coming from overseas.
Who should get vaccinated for mpox in Australia?
Eligible people can access mpox vaccines for free in Australia.
Vaccination is recommended for men who have sex with men, sex workers, and healthcare and laboratory staff at risk of exposure.
Those who have close physical contact with an infected person or are immunocompromised is also considered high risk.
Anybody at risk who is planning to travel to a country experiencing a significant outbreak should be vaccinated four to six weeks before travelling.
The best time for people to receive the vaccine is before they are exposed to mpox.
Eligible groups can be vaccinated for free with no Medicare card required.
Almost 23,000 vaccinations have been administered in Australia since January, according to data from the Australian Immunisation Register.
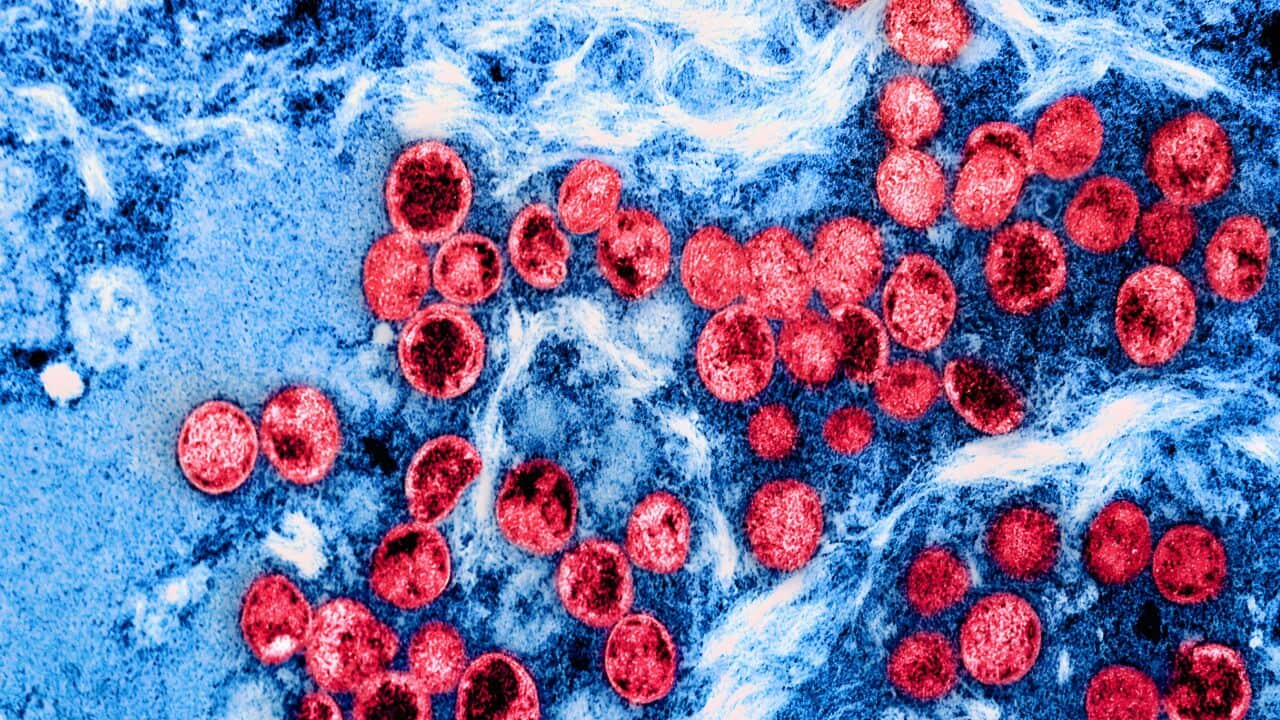
What is mpox?
Mpox is a viral zoonotic disease, and comes from the same family as the one responsible for smallpox.
Signs and symptoms can include a distinctive rash or lesions, swollen lymph nodes, headache or fever, muscle aches, joint pain, back pain, chills and exhaustion.
The virus can be transmitted through intimate or prolonged physical contact, close contact with rashes on the skin, body fluids (including droplets from coughing or sneezing) and contaminated objects such as linen and towels.
Symptoms typically clear after two to four weeks for most people, but some can become seriously ill.
There are two major variants of mpox; clade 1 and clade 2. Clade 1 typically causes more serious illness, while clade 2 is a less severe infection.
The cases in Australia are a variant of clade 2.
Associate Professor Oyelola Adegboye, from the Menzies School of Health Research at Charles Darwin University, said while the variant in Australia is less serious than some overseas, it should be taken seriously.
He said anybody at risk of contracting the virus should get vaccinated.
"I don't think this disease is going anywhere... there will be outbreaks on and off, and that's why people that are at risk or work in the (medical) area should get vaccinated and be prepared," he said.
"If the 1b does show up in Australia, that would be really concerning because it is highly infectious and serious."
Mpox was declared a global health emergency in August as a new strain called clade 1b began spreading from the Democratic Republic of Congo to neighbouring countries.
The strain is considered more deadly and more transmissible but is not believed to have yet reached Australia.