Key Points
- Australia's national science agency has warned about the rise of antimicrobial resistance (AMR) and superbugs.
- If left unchecked, it's estimated that AMR will be responsible for 10 million deaths annually by 2050.
- So what is AMR, how dangerous are superbugs, and what can Australia do to prevent the rise of infections?
There are fears a "silent pandemic" of antimicrobial resistance, resulting in superbugs, could kill millions globally within decades and has prompted a plea for greater action in Australia.
A new damning report released by on Tuesday warned that Australia must act promptly if it does not want to be thrust back to a time when simple infections can prove deadly.
The World Health Organization has If unchecked, it's estimated to kill up to 10 million people annually by 2050 and leave 24 million people in extreme poverty in the next decade.
So what are superbugs, how risky are they and what can be done to prevent being infected?
What is antimicrobial resistance?
Antimicrobial resistance, or AMR, refers to when antimicrobials - medicines used to prevent and treat infections - are no longer effective.
Without medicines like antibiotics or antivirals, it would make it difficult or even impossible to treat illnesses - rendering humans at serious risk of being defenceless to serious conditions.
The overuse - or misuse of antibiotics - can lead to medication becoming ineffective against certain bacteria and other microbes, meaning even simple infections or surgeries become extremely risky.
Medical procedures, from caesarian sections or hip replacements to cancer chemotherapy, will all become more threatening with AMR.
What are superbugs?
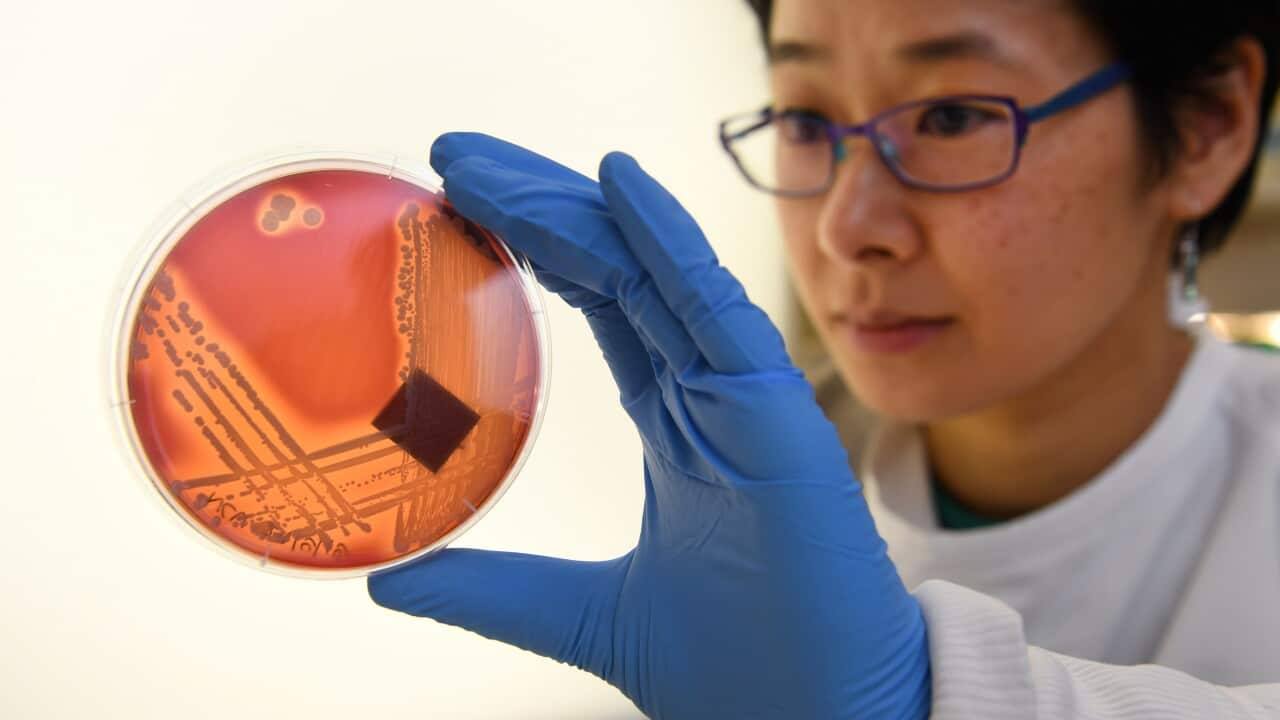
As AMR becomes an increased concern, so-called superbugs have become a serious risk as well. Superbugs are forms of bacteria that are resistant to all available treatments and can cause life-threatening infections.
They have the potential to spread among living things in health and agricultural settings before they make their way to humans and animals, causing "significant harm", according to the CSIRO report.
The report also reiterated the concerns in a United Nations report released earlier this month that superbugs could be responsible for 10 million deaths every year by 2050, potentially costing the global economy $148 trillion.
How dangerous can they be?
About 5,000 deaths each year in Australia and more than 1.27 million deaths around the world are linked to AMR, according to the CSIRO report that offered solutions to the looming health crisis.
Research from the national science agency and the Australian Academy of Technological Sciences highlights the need for better coordination to tackle the problem, which has been described as a "silent pandemic".
"AMR has the ability to render some of the most critical antimicrobial drugs ineffective," the report said.
"Losing effective antimicrobial treatments against infections would be catastrophic for health."
What can be done to combat it?
Greater emphasis needs to be placed on commercial sectors stepping in with advanced technology, rather than the discovery of new antibiotics, the research says.
It calls for better surveillance systems, vaccine production and diagnostic practices, as well as the prevention of the spread of superbugs through improved design of high-risk settings like farms and hospitals.
Examples include toilets that sense and deal with harmful microbes before they reach waterways, or surface sprays that change colour if a pathogen is present.
"[Antimicrobial resistance] could render some of the most critical antimicrobial drugs ineffective, undermining modern medicine and making us vulnerable to drug-resistant infections," according to lead author Branwen Morgan from the CSIRO.
"This report calls out the key challenges and opportunities for Australia to improve how we prevent, detect, diagnose and respond to drug-resistant infections and reduce the impacts."
Can they be treated?
Research is already underway into new types of antibiotics, but it's feared that alone will not be enough.
Other recommendations included creating a central body to track antimicrobial resistance, developing national policy and standards and ramping up public messaging.
"[Antimicrobial resistance] doesn't respect national, state, or sectoral boundaries," the report said.
"It is critical that solutions are designed from a 'one health' perspective, acknowledging the undeniable interplay between humans, animals and the environment.
"This will be key to making sure that in creating a solution for one sector, a problem is not being generated for another."
Additional reporting by Rayane Tamer