Highlights
- Cancer Australia says people with cancer are at an increased risk of more severe infection if they contract COVID-19.
- People with cancer have not been included in clinical trials.
- Cancer Australia says although researchers are still building up the evidence, vaccines are likely to be effective for people with cancer.
SBS asked Cancer Australia why the body is encouraging people who have cancer to get vaccinated and how vaccines would interact with cancer treatments.
In this Q&A, Professor Dorothy Keefe, CEO of Cancer Australia, answers some key questions.
Why should people with cancer get vaccinated?
Professor Keefe: People with cancer are more vulnerable to contracting COVID-19, and if they get COVID-19, they are at an increased risk of more severe infection. Getting a COVID-19 vaccine is a safe and effective way for people with cancer to protect themselves, their family, and their community against COVID-19.
Most people affected by cancer (and their carers) are eligible to receive a COVID-19 vaccine now as part of the Australian Government’s COVID-19 vaccine national roll-out strategy.
Even after receiving a COVID-19 vaccine, it is still important for people with cancer (and all people in Australia) to continue to protect themselves against COVID-19. This includes wearing a mask, washing hands with soap and water, using hand sanitiser, and maintaining physical distancing.
Is it safe for people with cancer or people who have a weaker immune system to get the COVID-19 vaccines?
Professor Keefe: Currently, there are no unique concerns about the safety of either of the COVID-19 vaccines available in Australia (the Pfizer and AstraZeneca vaccines) in people with cancer or people who are immunocompromised.
Whilst people with cancer were not included in the initial clinical trials for the COVID-19 vaccines, based on a general understanding of the vaccines and information being collected from COVID-19 vaccination programs internationally, there are no significant safety issues specific to people with cancer receiving the COVID-19 vaccines.
Why weren’t people with cancer included in clinical trials for the COVID-19 vaccines?
Professor Keefe: People with cancer were not included in the initial clinical trials for the COVID-19 vaccines because clinical trials typically need to see whether the vaccines will work in people with healthy immune systems before they are trialled in people who are immunocompromised.
Is any data being collected about the COVID-19 vaccines for people affected by cancer?
Professor Keefe: Yes, data is being collected nationally and internationally to understand the use of the COVID-19 vaccines in people with cancer.
This data will help us better understand the safety and efficacy of the vaccines for people with cancer, as well as more specific information such as how different treatments impact vaccine responses, how patients with different types of cancers respond to the vaccines, and the impact of timing of the vaccine for patients on cancer treatments.
We at Cancer Australia are monitoring this and will continue to update our as information becomes available.
Additionally, Cancer Australia has established an important clinical study, , to better understand the safety and efficacy of the COVID-19 vaccines in people with cancer in Australia, including in people with solid tumours and blood (haematological) cancers.
Should people with allergies avoid any of the COVID-19 vaccines?
Professor Keefe: People who have had an allergic reaction or a severe allergic reaction (anaphylaxis) to any ingredients contained in the COVID-19 vaccines should avoid the specific vaccines that contain those ingredients.
Allergies of particular relevance to people with cancer include allergies to polysorbate 80, which is one of the ingredients in the AstraZeneca vaccine, and polyethylene glycol (PEG), which is one of the ingredients in the Pfizer vaccine.
These ingredients are also used in cancer treatments, such as chemotherapy medications, docetaxel and paclitaxel.
If you have had an allergic reaction or anaphylaxis in response to polysorbate 80 or PEG, speak to your health professional or seek expert advice on COVID-19 vaccination before being vaccinated.
What are the side effects of the COVID-19 vaccines for people affected by cancer?
Professor Keefe: Common side effects from the COVID-19 vaccines are similar to side effects of other vaccines, including pain, redness and/or swelling where you received the needle, muscle pain/aches, mild fever, headache, or tiredness.
A very rare side effect of blood clotting called thrombosis in combination with thrombocytopenia syndrome (or TTS) has been reported after COVID-19 Vaccine AstraZeneca. Currently, there is no evidence to suggest that people affected by cancer will experience different or worse side effects to the COVID-19 vaccines than other people.
Will the COVID-19 vaccines affect or interact with the cancer treatment(s)?
Professor Keefe: Currently, there is limited information available from COVID-19 vaccines clinical trials about whether the COVID-19 vaccines will affect or interact with cancer treatments.
If you are having or have had treatment for cancer, speak to your healthcare team about the best timing for you based on your own situation.
Factors to consider include the type of cancer you have/had, the type and timing of your treatment, which vaccines are available to you, and how your immune system is working.
Do the COVID-19 vaccines work for people affected by cancer (are they effective)?
Professor Keefe: Although researchers are still building the evidence about how well the COVID-19 vaccines work for people affected by cancer, there is a lot of similar evidence from other vaccines that suggests the COVID-19 vaccines are likely to be effective for people affected by cancer.
For example, evidence from flu vaccinations suggests that people affected by cancer can mount a protective immune response from COVID-19 vaccines, and evidence from other vaccines used to prevent infection suggests COVID-19 vaccination will be effective for people affected by cancer, even in those who are undergoing immunosuppressive therapy.
With that said, for people who are immunocompromised, the immune response to any vaccine may be reduced, which means they may have less protection compared to people who are not immunocompromised.
This is one of the reasons why it is important for people affected by cancer and their close contacts to continue taking other protective measures against COVID-19 even after they have received the vaccine.
Where and when can people affected by cancer receive their COVID-19 vaccine?
Professor Keefe: For people affected by cancer, decisions about where and when to receive the COVID-19 vaccine can be made on an individual basis by the person with cancer together with their healthcare team.
In general, the vaccines are available through participating General Practitioners (GPs), Aboriginal Community Controlled Health Services, Commonwealth Vaccine Clinics, pharmacies and State and Territory vaccination clinics.
You can find vaccination locations and book an appointment using the Australian Government’s . This has now also been translated into several languages.
Who will administer the COVID-19 vaccines to people with cancer?
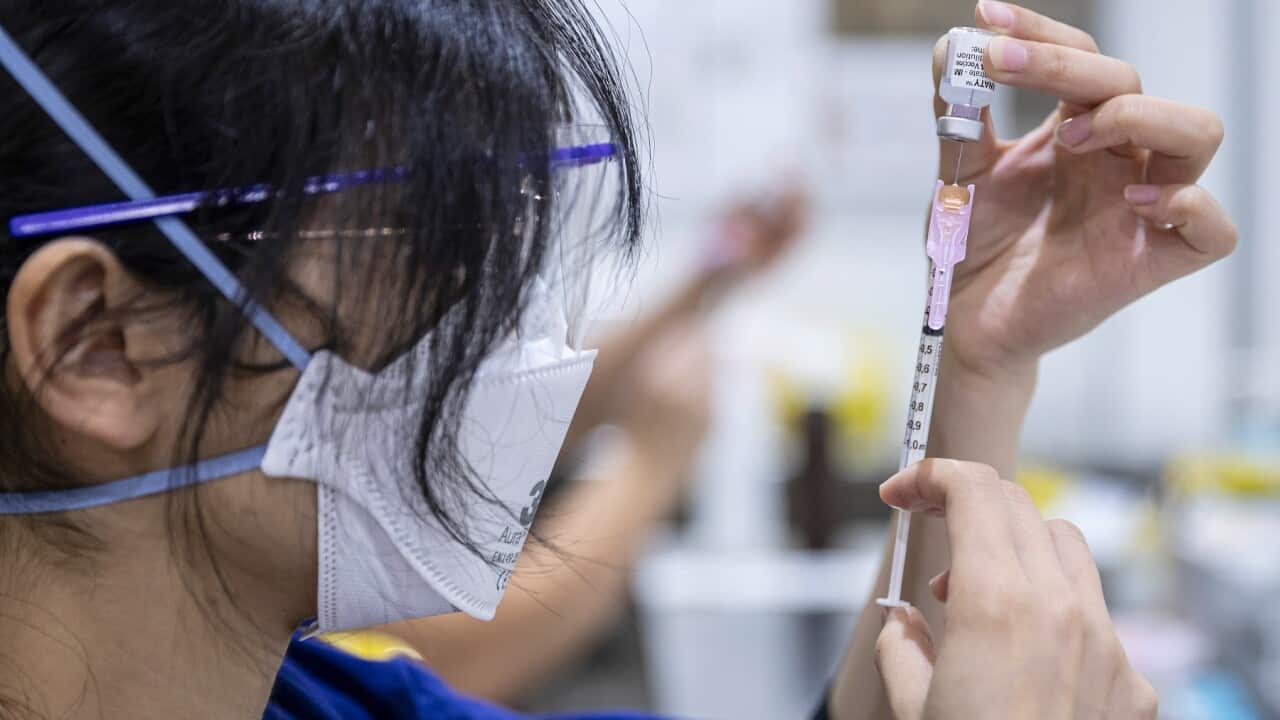
Professor Keefe: Only qualified healthcare professionals can administer the COVID-19 vaccines.
Additionally, every healthcare professional who administers the COVID-19 vaccines must complete compulsory COVID-19 vaccination training, which covers important information, including the handling and administration of COVID-19 vaccines.
For people affected by cancer, this may affect whether their healthcare team can administer the vaccine to them directly or whether they will need to go to another approved vaccine provider.
Will people with cancer receive a different COVID-19 vaccine or a different dosage from other people?
Professor Keefe: People with cancer are offered the same COVID-19 vaccines and the same dosages as the rest of the Australian population.
Currently, both vaccines available in Australia (Pfizer and AstraZeneca) require two doses, and it is important for all people to get the recommended dosage of the COVID-19 vaccine they are offered. However, this may be particularly important for people with cancer.
This is because studies using the Pfizer vaccine found that some cancer patients had lower levels of protection against COVID-19 following the first dose of the vaccine compared to people without cancer.
However, when cancer patients received their second dose three weeks after the first dose, protection improved significantly.
This is another one of the reasons why it is important for people affected by cancer and their close contacts to continue taking other protective measures against COVID-19, such as wearing a mask, washing your hands and maintaining physical distancing, even after they have received the vaccine.
Cancer Australia has published some in 10 languages: Arabic, Chinese (Simplified), Chinese (Traditional), Greek, Hindi, Italian, Korean, Spanish, Tagalog, and Vietnamese.
Cancer Australia has also developed with cancer.
Quarantine, travel, testing clinics and pandemic disaster payment
Quarantine and testing requirements are managed and enforced by state and territory governments:
If you want to travel overseas, you may be able to apply online for an exemption. for more information about the conditions to leave Australia. There are temporary measures for international flights that are regularly reviewed by the government and updated on the website.
- News and information over 60 languages at
- Relevant guidelines for your state or territory: , , , , , , .
- Information about the .
Visit the translated resources published by NSW Multicultural Health Communication Service:
Testing clinics in each state and territory:
Pandemic disaster payment information in each state and territory: